Scaly patches on face, hands and arms can indicate conditions ranging from dry skin to eczema, psoriasis or precancerous lesions. Seek medical attention for persistent, changing, bleeding or painful patches.
- Dr Sharon Crichlow
- Reading Time: 10 Mins
Rough, scaly patches on your skin can be irritating, unsightly and sometimes concerning. These patches range from simple dry skin to signs of more serious conditions. Most are harmless and treatable, but some require medical attention. Knowing what’s causing your scaly skin and recognising when to seek help can prevent complications and provide relief.
Key Takeaways
- Most scaly patches result from common conditions like dry skin, eczema, or psoriasis, but some may indicate precancerous lesions requiring medical attention.
- Monitor patches that change in size, shape, or colour, especially on sun-exposed areas like face, hands, and arms.
- Early treatment with proper moisturization, trigger avoidance, and sun protection can prevent complications and reduce discomfort.
Table of Contents
What Are Scaly Patches on the Face, Hands and Arms?
Scaly patches are areas where the skin becomes rough, flaky, and sometimes raised. They often feel dry to the touch and may appear red, white, or silvery depending on the underlying cause.
These patches commonly appear on the face, hands, and arms because these areas receive the most sun exposure and environmental contact. Unlike the skin on other body parts, these areas are rarely covered, making them vulnerable to UV damage, weather extremes, and various irritants.
The appearance of scaly patches can range from small, isolated spots to larger areas of affected skin. They may be temporary or chronic, and can sometimes be an early warning sign of more serious conditions.
What are the Main Causes of Scaly Patches
Several different conditions can cause scaly patches on exposed skin areas. Each has distinctive characteristics that can help identify the underlying cause.
Actinic Keratosis (Sun-Damage Spots)
Actinic keratosis (AK) develops primarily on sun-exposed areas like the face, hands, and forearms. These rough, scaly patches result from years of cumulative UV exposure.
Research by Guorgis et al. (2020) confirms that chronic UV damage is the primary cause of these lesions. They typically appear as small, rough spots that may be red, tan, pink, or flesh-colored.
What makes actinic keratosis particularly important to identify is its potential to develop into squamous cell carcinoma, a type of skin cancer. According to Balcere et al. (2022), lesions that persist for long periods or merge into larger patches carry a higher risk of progression to invasive carcinoma.
People with fair skin, those who work outdoors, or individuals with a history of significant sun exposure are at higher risk for developing these precancerous lesions.
Eczema
Eczema (atopic dermatitis) causes inflamed, itchy, and scaly skin patches. On the hands, eczema can be particularly troublesome and is quite common.
These patches typically appear red and inflamed on fair skin, while on darker skin tones, they may appear brown, purple, or grey. The affected areas often become extremely itchy, especially at night.
Common triggers include:
- Frequent hand washing
- Exposure to harsh chemicals
- Allergens like certain foods or pollen
- Stress
- Cold, dry weather
Psoriasis
Psoriasis creates thick, silvery-scaled patches on reddened skin. These patches most commonly appear on elbows, knees, scalp, and the lower back, though they can affect any body area, including the face and hands.
Unlike eczema, psoriasis patches tend to have more clearly defined edges and thicker scaling. The scales often have a distinctive silvery-white appearance sitting on top of red, inflamed skin.
Psoriasis is an autoimmune condition where the body accelerates skin cell production, causing cells to build up rapidly on the skin’s surface. It tends to run in families and may be triggered by stress, infections, or injuries to the skin.
Dry Skin (Xerosis)
Simple dry skin (xerosis) is an extremely common cause of scaly patches, particularly during winter months or in dry climates.
The skin on the hands and face is particularly vulnerable to dryness because these areas:
- Are frequently washed
- Have fewer oil glands than other body areas
- Are constantly exposed to environmental elements
Dry skin typically appears flaky and rough but lacks the inflammation seen in conditions like eczema or psoriasis. It might feel tight, especially after washing, and can become itchy and uncomfortable.
Contact Dermatitis
Contact dermatitis occurs when skin reacts to something it touches, creating scaly, irritated patches. There are two types:
Irritant contact dermatitis results from direct damage to the skin by harsh substances like cleaning products, soaps, or even frequent water exposure. A study by Huang et al. (2020) found that among healthcare workers, frequent hand washing was a significant risk factor for developing hand eczema with scaling and itching.
Allergic contact dermatitis is triggered by an allergic reaction to substances like nickel, fragrances, preservatives, or plants like poison ivy. The reaction typically develops 24-72 hours after exposure.
The resulting patches are often red, itchy, and scaly, appearing specifically in areas that contacted the triggering substance.
| Condition | Appearance | Common Locations | Key Characteristics |
|---|---|---|---|
| Actinic Keratosis | Rough, scaly patches; red, tan, or pink | Sun-exposed areas (face, hands, arms) | Can become precancerous; rough to touch |
| Eczema | Red, itchy patches with possible weeping | Hands, inside elbows, face | Intensely itchy; may crack and bleed |
| Psoriasis | Thick, silvery scales on red plaques | Elbows, knees, scalp, can appear on face/hands | Well-defined edges; thick scaling |
| Dry Skin | Flaky, rough patches without inflammation | Anywhere, common on hands and face | Improves with moisturising; seasonal |
| Contact Dermatitis | Red, scaly patches with distinct borders | Where contact occurred | Resolves when trigger is removed |
When to See a Dermatologist for Scaly Patches
You need to seek prompt medical attention if patches bleed, become painful, or develop ulcers. Don’t delay evaluation for patches that change rapidly in size, shape, or colour, especially on sun-exposed areas.

Our dermatologists in Hertfordshire specialise in diagnosing and treating various skin conditions, including persistent scaly patches that require professional evaluation.
How to Monitor Scaly Patches at Home
Keep track of any skin changes between medical appointments:
- Take clear, well-lit photos of affected areas weekly
- Note any changes in size, colour, texture, or associated symptoms
- Record potential triggers (new products, stress, weather changes)
- Document which treatments help or worsen the condition
This information will be valuable when consulting with healthcare professionals.
| Monitoring Aspect | What to Record |
|---|---|
| Appearance | Size, colour, texture (rough, smooth, raised, flat) |
| Symptoms | Itching, pain, bleeding, cracking (rate severity 1-10) |
| Triggers | New products, foods, activities, stress levels |
| Treatments | Products used, frequency, effectiveness |
Risks of Leaving Scaly Patches Untreated
Neglecting persistent scaly patches can lead to several complications.
For actinic keratosis, research shows a 5-10% risk of progression to squamous cell carcinoma. Longstanding patches have an increased likelihood of malignant transformation.
Untreated eczema can lead to skin infections if scratching breaks the skin barrier. Chronic inflammation may also increase stress and affect sleep quality.
Even simple dry skin, if severely neglected, can crack deeply enough to allow bacteria entry, potentially causing infections requiring antibiotics.
The psychological impact shouldn’t be overlooked either, as visible skin conditions can affect confidence and quality of life.
Simple Care Tips to Protect and Soothe Your Skin
While medical treatment is often necessary, simple measures can help manage scaly patches.
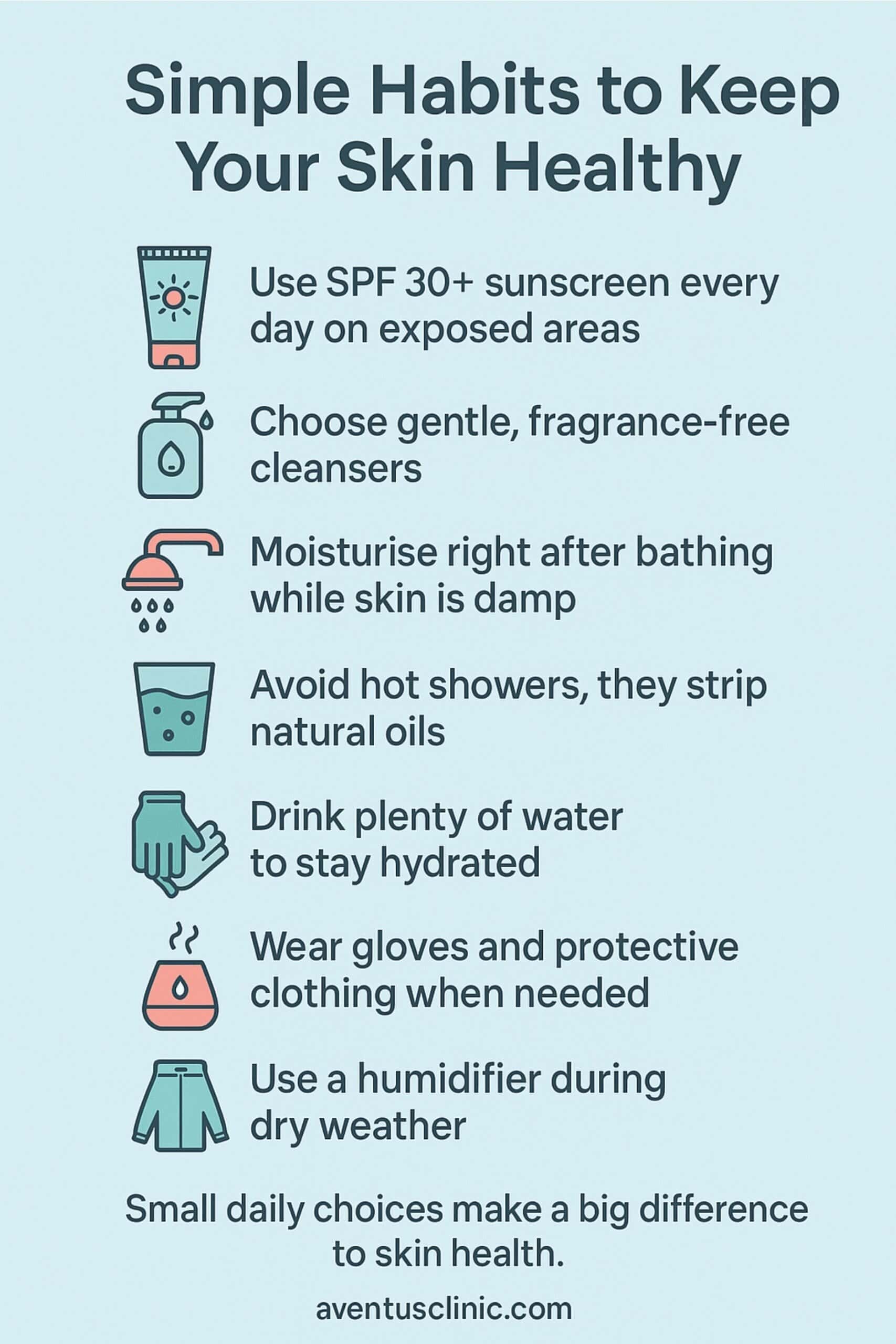
For specific conditions, targeted approaches help. Like, for eczema-prone skin, the research by Ghezzi et al. (2025) recommends using thick emollients and avoiding known triggers.
For actinic keratosis prevention, sun protection is essential according to multiple studies.
Conclusion
Scaly patches on your face, hands, and arms usually indicate common, treatable skin conditions. However, persistent patches, especially those that change or appear on sun-exposed areas, warrant professional evaluation.
If you’re concerned about persistent scaly patches, don’t hesitate to seek expert advice. We offer free online assessments to help determine the nature of your skin condition and provide appropriate treatment recommendations. Early intervention ensures better outcomes and peace of mind.
FAQ
Do scaly patches always mean skin cancer?
No. While some scaly patches like actinic keratosis can potentially develop into skin cancer, most scaly skin conditions are non-cancerous. Common causes include dry skin, eczema, and psoriasis. However, persistent or changing patches should be evaluated by a doctor.
How do I tell the difference between eczema and psoriasis?
Eczema typically causes red, itchy patches that may weep or crust. Psoriasis produces thicker, silvery-white scales on well-defined red plaques. Psoriasis scales are typically thicker, while eczema tends to be more intensely itchy. A dermatologist can provide a definitive diagnosis.
Can actinic keratosis heal on its own?
Some actinic keratosis lesions may temporarily regress, but most persist or progress without treatment. According to research by L.O. Guerra et al. (2024), while some lesions may regress naturally, many remain or worsen over time, potentially developing into skin cancer.
Do scaly patches get worse in winter or dry weather?
Yes, most scaly skin conditions worsen in cold, dry weather. Lower humidity levels draw moisture from the skin, exacerbating dryness and scaling. Heating systems further reduce indoor humidity. Increased moisturising and using a humidifier can help manage symptoms during these periods.
Should I worry about scaly patches on my hands or face more?
Both locations warrant attention, but for different reasons. Face patches are more visible and may cause psychological distress. Hand patches may crack more easily due to frequent washing and exposure. Sun-exposed areas like the face and hands also have higher risk for actinic keratosis.
When does a scaly patch need a biopsy?
A biopsy may be recommended if a patch shows warning signs like rapid growth, irregular borders, bleeding, or unusual colours. Your doctor might also suggest a biopsy if the patch doesn’t respond to standard treatments or if there’s suspicion of skin cancer or a rare skin disorder.

Book Your Free Skin Assessment
Persistent or changing scaly patches on your face, hands, or arms may signal underlying skin conditions. Get expert advice and personalised treatment options from our dermatology specialists today.









 WHATSAPP
WHATSAPP